Embryonic and adult stem cells
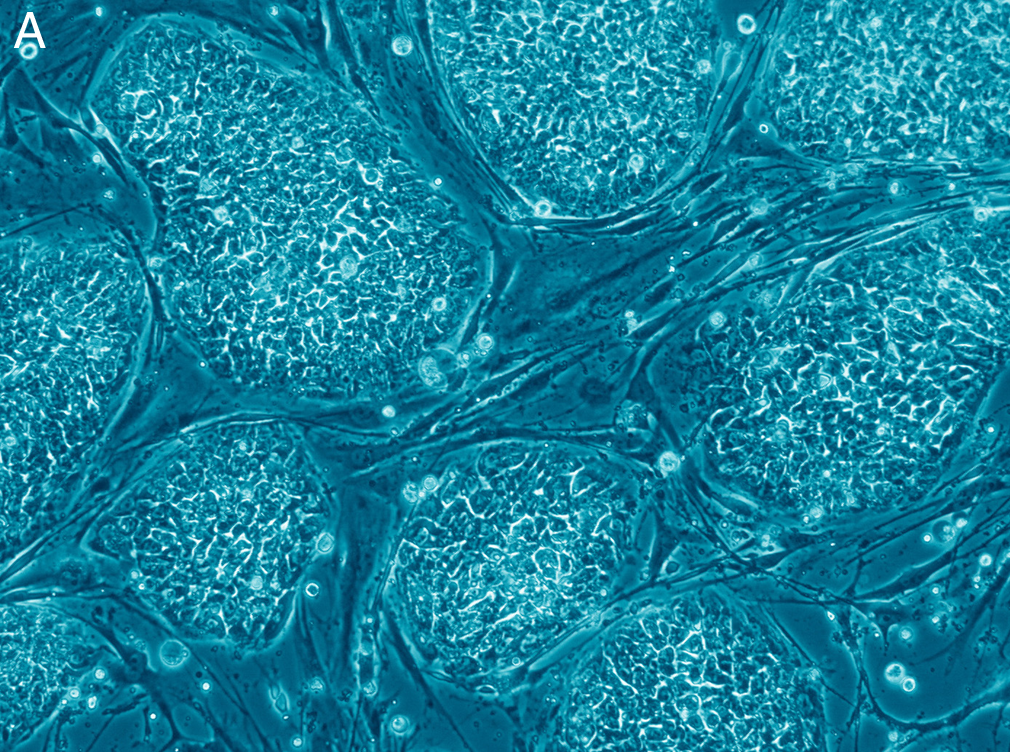
Stem cells are cells that provide new cells during growth, and replace cells that are damaged or lost during life. They have the following two important properties that enable them to do this:
- The ability to develop (differentiate) into many other, different cell types, for example brain cells, heart cells or liver cells.
- The capacity to replicate (self-renewal) and generate more of these important cells.
Mammals have two types of stem cells; embryonic stem cells (ESCs) and adult stem cells. ESCs are derived from an early-stage embryo, while adult stem cells are found throughout the body after development. The main difference between these cells is their ability in the number and type of different cell types they can become. Embryonic stem cells are pluripotent, meaning that they can become all cell types. Adult stem cells are multipotent and can only develop into a limited set of cell types.
Induced pluripotent stem cells
In 2006, the lab of Shinya Yamanaka showed that mouse skin cells could be converted into stem cells by using four specific factors, the Yamanaka factors (1). These cells were named “induced pluripotent stem cells (iPSC). For this important finding Yamanaka was awarded the 2012 Nobel Prize together with Sir John Gurdon. One year later a similar strategy was used to successfully reprogram human skin cells into human iPSCs (2). Nowadays, these iPSCs are an important tool in biomedical research and used for disease modelling, to study disease mechanisms, for drug development and cell replacement studies. To model a disease, a skin biopsy or a urine sample from a patient can be used to generate patient-specific iPSCs. Another option is to modify iPSCs using CRISPR/Cas9. Using defined protocols, these iPSCs can be converted into, for example, brain cells or even mini brains (organoids), which can be used to study a disease. Furthermore, when differences (phenotypes) are found in these cultures, this can be used to screen for drugs that reverse this particular aspect of the disease.
Stem cell-based therapies for SCA
A last aspect is that these iPSCs can be used to replace damaged or lost cells. Since the first stem cell-based clinical trials to replace brain cells that are lost in Parkinson Disease, stem cell replacement therapy has evolved and numerous clinical trials were initiated. In the spinocerebellar ataxia (SCA) field, the first preclinical experiment of embryonic transplants into a mouse model of SCA1 showed a positive effect on animal behaviour and brain pathology (4). Although these first preclinical experiments in SCA disease models are positive, an iPSC-based therapy for SCAs is far from a clinical application.
If you would like to learn more about stem cells, take a look at these resources by the National Ataxia Foundation and National Institutes of Health.
Snapshot written by Dr. Ronald A.M. Buijsen and edited by Frida Niss.
References
- Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126(4):663-76.
- Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131(5):861-72.
- Mandai M, Watanabe A, Kurimoto Y, Hirami Y, Morinaga C, Daimon T, et al. Autologous Induced Stem-Cell-Derived Retinal Cells for Macular Degeneration. The New England journal of medicine. 2017;376(11):1038-46.
- Kaemmerer WF, Low WC. Cerebellar allografts survive and transiently alleviate ataxia in a transgenic model of spinocerebellar ataxia type-1. Exp Neurol. 1999;158(2):301-11.









