Written by Jorge Diogo Da Silva Edited by Dr. David Bushart
Normalizing neuronal dysfunction in SCA3/MJD by activating a receptor inside cells
Spinocerebellar ataxia type 3 (SCA3), also known as Machado-Joseph disease (MJD), is an inherited neurodegenerative disease that typically begins in mid-adulthood. This disease causes loss of coordination and balance (a group of symptoms known as ataxia), abnormal eye movements, and other motor symptoms, all of which limit a patient’s daily life activities. Treating SCA3 patients is currently very challenging, since there are no drugs or other treatments that slow or stop the progression of this disease. While several therapeutic options have been tested in clinical trials, none have shown considerable and consistent effects in improving disease symptoms. Therefore, it is imperative that other treatments are investigated and tested in the clinical setting, in the hopes that we might find a way to improve the lives of SCA3 patients.
The cause of this disease is very well-characterized: patients with SCA3 have an abnormal form of a protein called ataxin-3. All proteins are made up of a sequence of several smaller building blocks known as amino acids. In ataxin-3’s sequence, there is a region where one type of amino acid, glutamine, is repeated consecutively. SCA3 arises when the number of these repeated amino acids is very high (an abnormality known as a polyglutamine expansion), which is toxic for cells.
One of the regions of the brain that is most responsible for regulating balance and movement coordination is the cerebellum, which is located just behind the brainstem (the region connecting the spinal cord to the rest of the brain). As expected, the cerebellum is one of the most affected brain regions in SCA3, since it helps control gait and coordination. Purkinje cells, which are some of the largest neurons in the brain, make up a substantial portion of the cerebellum. These cells receive information from other neurons that detect our surroundings, then emit a signal to the brain regions that control muscles and regulate our movement. This allows us to make movements that are coherent and fluid.
Since Purkinje cells are dysfunctional in SCA3, it is reasonable to think that improving the well-being of these cells could also reduce symptoms. In a recent publication, Watanave and colleagues described how they explored a strategy to improve Purkinje cell function using drugs in a mouse model of SCA3, with findings that could be relevant for future studies in patients.
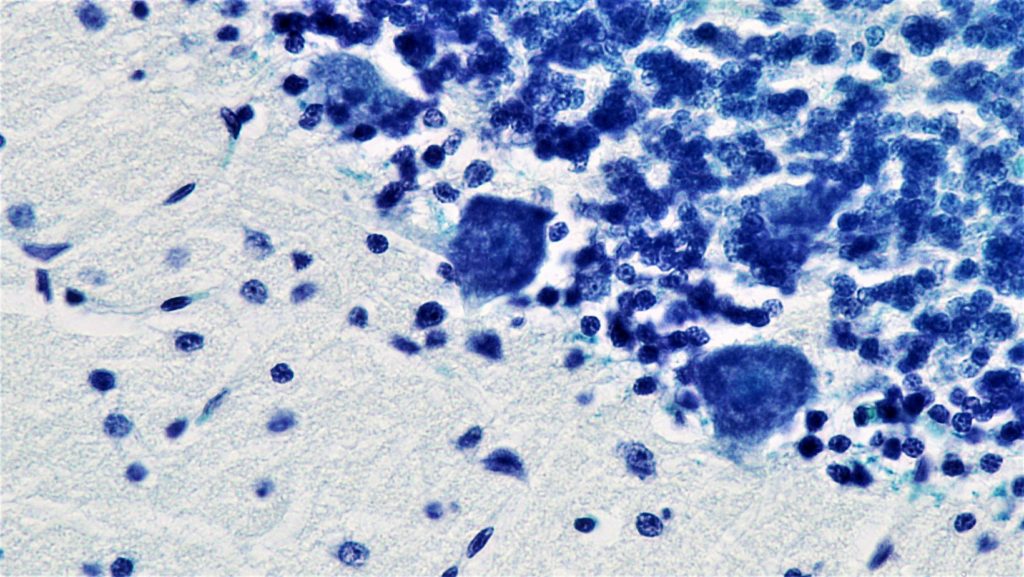
First, SCA3 mice were generated by injecting the ataxin-3 protein with a polyglutamine expansion directly into the cerebellum, which was done using a system that allows delivery of proteins into neurons. This procedure causes mice to develop motor symptoms similar to SCA3 patients. In addition, certain properties of Purkinje cells are severely affected by the injection of expanded ataxin-3: the researchers found that the structure of these neurons is abnormal, as is their function (that is, their ability to receive and emit signals from and to other neurons). Additionally, they also observed a deficiency in proteins other than ataxin-3 that are important for Purkinje cell signal transmission and health. By doing this initial analysis, the researchers were able to better understand their SCA3 mouse model. This allowed them to then establish a drug testing system in these mice that is both fast and reliable.
Using this new drug testing protocol, Watanave and colleagues tested two possible treatments for SCA3. The first one, named Ro0711401, is a drug that increases the activity of one of the proteins that was found to be deficient in the SCA3 mouse model: mGluR1. mGluR1 is a cellular receptor located in the membrane (the structure surrounding a cell) that is essential for the transmission of signals in Purkinje cells. Ro0711401 works by normalizing the function of mGluR1, which could possibly stabilize cells where this receptor is not working properly. In this study, the researchers found that Ro0711401 treatment was able to improve symptoms in SCA3 mice. Further studies will be needed to evaluate the effect of this drug, but these early results are promising.
The second drug that was tested was SR1078, which also activates a receptor: “retinoid-related orphan receptor α” (RORα). This receptor acts inside neurons and can change numerous processes that are important for signal transmission and overall cellular function. Interestingly, other types of ataxias are caused by mutations in RORα, potentially making it a good target for drug treatment. After treating SCA3 mice with SR1078, the team saw an improvement in symptoms, as well as a recovery of Purkinje cell structure and signal transmission properties. This makes SR1078 a very promising drug, since it improves symptoms by targeting one of the most highly affected cell types in SCA3. While more studies are needed, this drug might be able to normalize Purkinje cell function, which is especially important since Purkinje cell dysfunction is also a hallmark of several other forms of ataxia. Indeed, previous studies have shown that this drug may also improve Purkinje cell function in other diseases that have different underlying causes than SCA3.
In conclusion, Watanave and colleagues have proposed two drugs that are able to improve the symptoms of a mouse model of SCA3 by activating cellular receptors: one that is in the cellular membrane and one that is inside of cells. Not only are these results interesting from the perspective of improving symptoms, but also because of the cellular effects of the two drugs: there are certain problems in the structure and function of Purkinje cells that are associated with SCA3, and Ro0711401 and SR1078 normalize these specific defects. This provides hope for the development of specific treatments for SCA3 using these drugs. However, it is important to stress that Ro0711401 and SR1078 must be further tested in different mouse models to assess both their effectiveness and safety profile. Only then could they be used in a clinical trial with SCA3 patients.
Key Terms
SCA3/MJD: a hereditary neurological disorder of the adult mid-life whose main symptoms are the loss of balance while standing and walking, as well as a lack of motor coordination.
Polyglutamine expansion: an increase in the number of glutamine amino acids (the building blocks of proteins) that are consecutively present in a single protein, which can cause diseases such as SCA3. For more information, see our Snapshot on Polyglutamine Expansion.
Conflict of Interest Statement
The authors and editor declare no conflict of interest.
Citation of Article Reviewed
Watanave, M., et al., Pharmacological enhancement of retinoid-related orphan receptor α function mitigates spinocerebellar ataxia type 3 pathology. Neurobiology of Disease, 2018. 121: 263-273. (https://www.ncbi.nlm.nih.gov/pubmed/30343032)










