Written by Anna Cook Edited by Dr. Monica Banez
Researchers successfully use an existing multiple sclerosis drug to improve performance in an SCA6 mouse model
Spinocerebellar ataxia type 6 (SCA6) is a rare hereditary movement disorder affecting 5 of every 100,000 people worldwide1. The disease is caused by the expansion of a repeating DNA sequence in the CACNA1A gene. The length of this repeat, which is made up of sequential iterations of the code CAG, is normally variable in length, stretching between 4 and 18 repeats in the healthy population. However, in SCA6 patients, something goes wrong and the CAG repeat in the CACNA1A gene is expanded to have 21-33 repeats, causing dysfunction in the brain and motor symptoms for reasons that are not yet fully understood. SCA6 belongs to the group of disorders called polyglutamine diseases, all of which are caused by CAG expansions in different genes. These include disorders like Huntington’s disease and other spinocerebellar ataxias.
SCA6 onset generally occurs at middle age. The characteristic symptoms are difficulties with motor coordination that progressively get worse as patients get older. Current treatment options are limited to managing symptoms rather than addressing the cause of the disease. However, researchers have recently discovered that the FDA-approved drug 4-AP reduces motor symptoms in a mouse model of SCA6, making the drug a promising candidate for the treatment of the disease in humans.
To study disease in depth, many researchers use mouse models carrying the same genetic alteration that occurs in patients, which oftentimes recreates the causes and symptoms of the disease. In this study, the mice had been genetically altered so that their CACNA1A gene contained a CAG expansion mutation – the same mutation in the same gene that is found in SCA6 patients. These mice have motor deficits that start at 7 months (mid-adulthood in mouse years), which is later followed by degermation of Purkinje cells in the cerebellum. This time course – mid-life motor deficits followed by neurodegeneration later in life – mimics the progression of the disease in patients, making this model a promising starting point to investigate potential treatments.
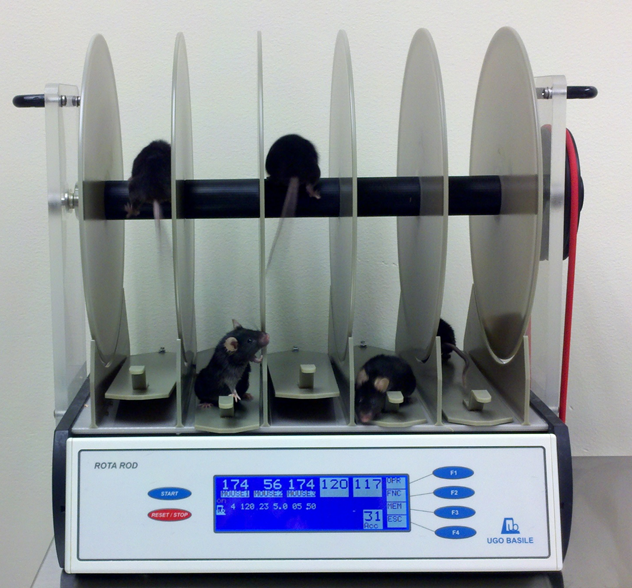
To test motor impairments caused by cerebellar abnormalities, researchers used a test called the rotarod. This consists of a rod that slowly rotates so that the mouse must work to not fall off. Managing the rotarod requires motor coordination skills, so measuring how long mice can stay on is a useful way to evaluate motor performance and reveal ataxia in mouse models. The SCA6 mice in this study performed much worse on the rotarod test than healthy mice did. Therefore, on a behavioural level, these mice proved to be a good model to study the motor dysfunction seen in SCA6. Then, to test 4-AP as a potential treatment for the motor abnormalities observed in SCA6, the researchers treated SCA6 mice by putting the drug in their drinking water. After one single week of treatment, the mice showed a dramatic motor improvement in the rotarod performance (though they were still not performing as well as the mice that lacked the SCA6 mutation). To determine how long this motor improvement lasted, researchers re-tested the treated SCA6 mice by withdrawing the drug and then testing a week later. They found that the motor improvement was reversed to the same performance level as non-treated mice. This meant that the 4-AP drug treatment effectively treated the motor deficits in the mouse model, but only as long as the treatment persisted.
Using the rotarod assay is not the only way for scientists to study ataxia in mice, however. In this case, the authors also looked at the some of the cells that are most affected in the brains of SCA6 mice. The most well-studied of these are the Purkinje cells, a type of large neuron in the cerebellum that is involved in motor coordination and functions abnormally in several ataxias, including SCA6. We also know from patient autopsies that Purkinje cells almost always show degeneration in human SCA6. By taking slices of brain tissue from the SCA6 mice, researchers could measure the activity of the Purkinje cells with an electrode. Normally these cells fire quickly and regularly, acting as pacemakers for our movements. However, in mice with the SCA6-causing mutation, Purkinje cells fired irregularly and more slowly, losing this pacemaker capacity. After seeing that the 4-AP treatment improved motor performance in the mice, researchers investigated whether the drug was doing this by correcting Purkinje cell firing. When they applied the drug directly to the brain slices, they found that Purkinje cells started firing more regularly. Although the rate of firing was still slower than is seen in healthy mice, the 4-AP was bringing pacemaker firing closer to normal.
In brain slices taken from the mice that had been treated chronically with 4-AP, firing deficits in Purkinje cells were also rescued. This improvement was seen in as little as a week after treatment was started. This partial rescue could explain why chronically-treated 4-AP mice performed better on the rotarod, though still not performing as well as healthy mice. In addition to brain slice recordings, researchers were also able to track the activity of Purkinje cells in living mice. This was done by inserting an electrode into the brain of anesthetised mice. Just like in slices, these recordings showed that SCA6 mice have decreased firing regularity, and that the chronic 4-AP administration rescued this deficit. More importantly, chronic administration for up to 3 months didn’t seem to have a detrimental effect in the motor performance or Purkinje cell firing activity in healthy mice. This means that 4-AP is likely a drug that is well-tolerated as a long-term treatment, suggesting that it could be used effectively to treat SCA6 over a patient’s lifetime.
This study shows that treating abnormal Purkinje cell firing in a mouse model of SCA6 can rescue abnormal motor behaviour. In addition, it also presents Purkinje cell firing as a target for future drug development. Interestingly, 4-AP is already used to treat multiple sclerosis 2 and can improve symptoms in patients with episodic ataxia type 2. Therefore, there is hope that this existing drug could be repurposed for the treatment of SCA6. Still, since these experiments were performed in a mouse model of SCA6, more research is needed to determine how effective the drug will be in ataxia patients – particularly to treat more advanced stages of the disease. Nevertheless, this is the first pharmacological intervention shown to work in any model of SCA6 and, as such, represents an exciting breakthrough in the treatment of this debilitating disease.
Key Terms
Rotarod: The rotarod is a technique that has been used for decades to test motor performance in mice and rats. Researchers place the animal on a rotating cylinder and record how long it takes for the animals to fall off as the rotation speed is gradually increased. The higher the mouse/rat’s motor performance, the longer they will be able to stay on.
Purkinje Neurons: A type of neuron in the cerebellum. They are some of the largest cells in the brain. They help regulate fine movement. Purkinje cell loss/pathology is a common feature in cerebellar ataxia.
Conflict of Interest Statement
Dr. Sriram Jayabal, who completed the work described in the summary is a contributor to SCAsource. Dr. Jayabal did not contribute to the writing or editing of this summary.
Anna Cook, who wrote this piece, is completing graduate work in the Watt lab where this work was carried out. Anna Cook did not contribute to the work described in the article.
The editor has no conflict of interest to declare.
Citation of Article Reviewed
Jayabal, S., Chang, H. H. V., Cullen, K. E., & Watt, A. J. (2016). 4-aminopyridine reverses ataxia and cerebellar firing deficiency in a mouse model of spinocerebellar ataxia type 6. Scientific reports, 6, 29489. https://www.nature.com/articles/srep29489
References
- Solodkin, A. & Gomez, C. M. Spinocerebellar ataxia type 6. Handb. Clin. Neurol. 103, 461–473 (2012).
- Davis, F. A., Stefoski, D. & Rush, J. Orally administered 4-aminopyridine improves clinical signs in multiple sclerosis. Ann. Neurol. 27, 186–192 (1990).










