
Snapshot: What is intelligibility?
Speech intelligibility refers to how many words can be correctly understood by a listener. For example, if someone says the phrase, “My name is John,” and a listener hears, “My Read More…
The Ataxia Community Comes Together in Orlando April 9–11, 2026 for the Annual Ataxia Conference! LEARN MORE
A collection of resources for individuals and families affected by Ataxia with Oculomotor Apraxia (AOA).
Ataxia with Oculomotor Apraxia (AOA) is caused by a genetic mutation that is passed on from parents to their children. AOA leads to problems with balance and coordination, as issues with moving eyes side to side. For complete information about symptoms, diagnosis, and treatment of Ataxia, visit our What is Ataxia? page. This page contains NAF’s resources that are specific to AOA.
Sign up for our mailing list to stay up-to-date on Ataxia news.
Presented by Brent Fogel, MD, PhD
During this webinar, Dr. Fogel looked at the causes and symptoms of Ataxia with Oculomotor Apraxia (AOA), the typical diagnostic journey for those affected, what to expect for clinical care, and an overview of current research into the disease.
NAF offers webinars on many topics to help you live better with Ataxia. Visit www.ataxia.org/webinars to find other helpful presentations.
Participating in a research study or clinical trial is one way to take an active role in furthering understanding and treatment of Ataxia. It is also a way to get access to new treatment options before they are widely available. To find studies that are enrolling patients, visit our Help Develop New Treatments page.
Ataxia with Oculomotor Apraxia (AOA) is a group of rare neurodegenerative disorders. There are many types of AOA, with the most common being AOA1, AOA2, and AOA4. Each type of AOA is caused by mutations in different genes.
SCAsource provides Ataxia research news, directly from researchers to the Ataxia community. Visit SCAsource to see their full collection. Here is a collection of articles relevant to AOA.

Speech intelligibility refers to how many words can be correctly understood by a listener. For example, if someone says the phrase, “My name is John,” and a listener hears, “My Read More…

Speech not only consists of the words we say, but how we say them. That “how” is what is called prosody: the pitch, loudness, and timing of speech. The term Read More…

Written by Ziyang Zhao Edited by Dr. Hayley McLoughlin A newly developed smartphone application will allow patients to assess ataxia at home. There’s an interesting problem in science that’s often Read More…
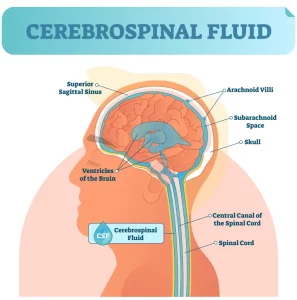
Public transit may not be the first thing that comes to mind when we think about the brain, but it’s a great way to understand how all the parts of Read More…
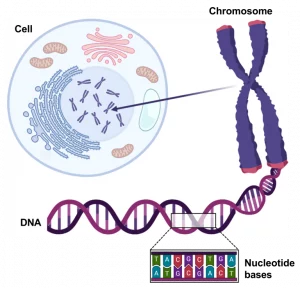
A gene is the basic physical unitof heredity. Every living cell contains genetic information that determines an organism’s development, form, and function. This genetic information is encoded by two macromolecules: Read More…
What is a recessive disorder? A recessive disorder is one that has a specific disease mechanism. For a recessive disorder to occur, both copies of the causative gene must be Read More…
