Written by Kim M. Gruver Edited by David Bushart
What’s cognition got to do with ataxia? Could the cerebellum mediate both cognitive and motor symptoms in the same disease? And how can scientists use mice to find out?
Spinocerebellar ataxia type 1, or SCA1, is a progressive neurodegenerative disease that has no cure. In SCA1, an expanded CAG repeat sequence in the ATXN1 gene increases the chain length of the amino acid glutamine (Q), so SCA1 is called a “polyQ” disease. As suggested by its name, the cerebellum is a heavily affected brain region in SCA1. Since the cerebellum is involved in motor coordination, it is no surprise that dysregulated control of movement, or ataxia, is a major symptom of SCA1.
However, what may come as a surprise is that some SCA1 patients also experience changes in cognition in addition to ataxia. Since the mutated ATXN1 gene is found throughout the brain, it has been difficult to tease apart whether the cerebellum contributes to the cognitive symptoms of SCA1 in addition to the motor symptoms. It is possible that cognitive symptoms of SCA1 might be exclusively caused by brain regions other than the cerebellum. For example, ATXN1 is also highly expressed in the prefrontal cortex, a region known for mediating many cognitive processes. But before we discount the possibility that the cerebellum plays a role in the cognitive symptoms experienced by some SCA1 patients, it is important to note an interesting observation in neuroscience research that has emerged in recent decades. Scientists have described a surprising role of the cerebellum in a host of neurological disorders like autism and schizophrenia. In light of these findings, that the cerebellum could be implicated in both the motor and cognitive symptoms of SCA1 may not be so far-fetched.
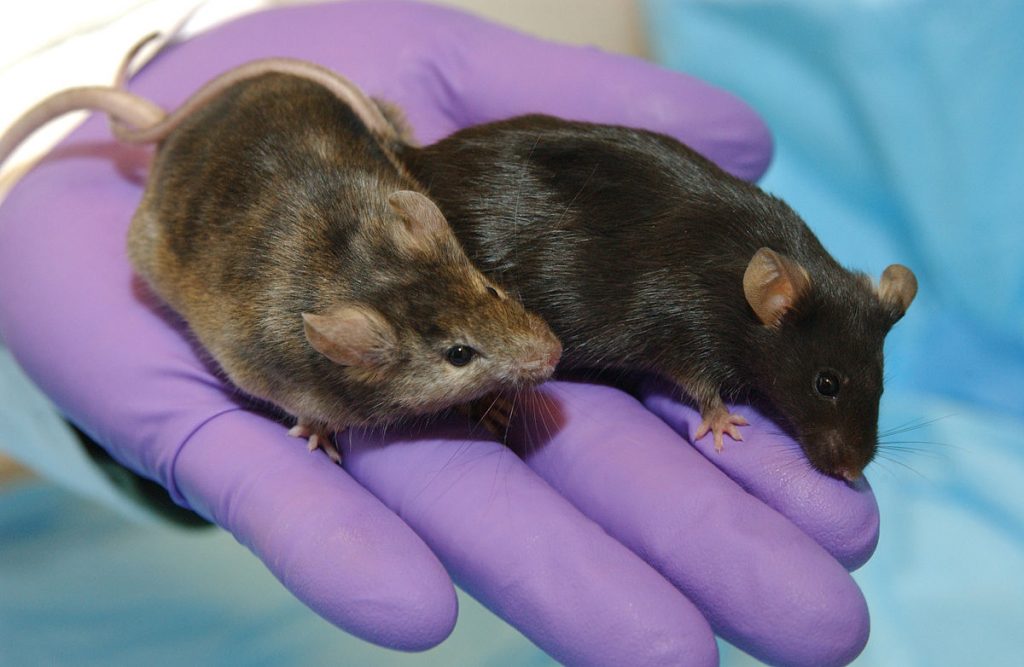
A powerful tool on the researcher’s lab bench to study diseases like SCA1 is the laboratory mouse. Since 1902, mice have played an indispensable role in disease research. Scientists can breed mice that express human genes, such as a mutated form of ATXN1, to figure out what goes awry in diseases like SCA1. Animal models of disease help researchers to identify potential treatment strategies that may be useful to humans. Since such in-depth analysis and careful experimental manipulation is impossible in human patients, animal models are an invaluable tool to study diseases like SCA1.
In the SCA1 field, scientists use multiple animal models to study SCA1. Researchers have harnessed the differences between these mouse models to address different questions, such as:
- “How does the number of CAG repeats affect SCA1 symptoms in mice?”
- “What happens if the ATXN1 gene is removed altogether?”
- “Do SCA1 symptoms still occur if the mutant ATXN1 gene is restricted to cerebellar Purkinje cells?
In mice and in humans, we know that the length of the polyQ expansion in the ATXN1 gene correlates with both the severity and the age of symptom onset of SCA1. Mice that express more CAG repeats (a longer polyQ expansion) in their ATXN1 gene experience more severe symptoms that start earlier in life than mice with a shorter polyQ expansion. When mutant ATXN1 expression is restricted to Purkinje cells in the cerebellum, mice display motor impairments similar to what is observed in mice with mutant ATXN1 expression everywhere in the brain. This tells us that disrupting healthy ATXN1 expression in Purkinje cells alone is sufficient to cause motor symptoms that stem from SCA1. To put it plainly, mouse models of SCA1 have been a crucial component of SCA1 research.
Since human SCA1 patients experience behavioral symptoms, scientists also use behavioral tools to evaluate the symptoms of SCA1 mice. Motor coordination tests are essential in ataxia research. These tests allow scientists to determine whether a potential intervention improves or worsens symptoms in mice. This is the first step to evaluate whether an intervention could be promising for human patients. However, as we discussed earlier, motor impairments are not the only symptom faced by SCA1 patients: many exhibit cognitive deficits as well. But could mice be used to evaluate something as complex as cognition? Can laboratory mice really help scientists uncover whether the cerebellum contributes to the cognitive impairments observed in SCA1? Researchers at the University of Minnesota say yes.
Asher and colleagues set out to answer the question of whether the cerebellum contributes to the cognitive impairments that have been observed in SCA1. The authors also highlight a path forward for using animal models to evaluate tricky questions like the nature of cognitive impairment in SCA1. In this study published in Human Molecular Genetics in January 2020, Asher et al. had two major goals: first, evaluate cognitive impairments across multiple SCA1 mouse models; second, determine whether the cerebellum contributes to cognitive impairments in a mouse model of SCA1.
Asher and colleagues were thorough and prudent: they bred mouse lines with the same genetic background and used them at the same age to reduce the number of variables that might confound their results. The authors also carefully chose behavioral assays to remove potential variables like stress from their data. Asher et al. assessed cognition in their SCA1 mouse models in ways that are relevant to a mouse: they assessed spatial learning using a test called the Barnes maze, and fear acquisition using contextual fear conditioning. For a mouse, learning how to navigate toward a hiding spot and to remember where to find it later can be the difference between life and death. Similarly, for a mouse to quickly identify and remember contexts where it experiences pain or danger is also relevant to its survival. Asher and colleagues tested multiple mouse lines that model SCA1 on two cognitive tests and compared the results. The researchers used mice that harbor a very long polyQ expansion in the ATXN1 gene expressed throughout the entire brain (154 CAG repeats, called “154Q mice”), mice that harbor a mild polyQ expansion (78Q mice), and mice with an increased polyQ expansion that is found only in cerebellar Purkinje cells (82Q mice). Asher et al. also evaluated the behavioral results from mice whose ATXN1 gene was either completely removed (a complete ATXN1 knock-out), or where one of the two inherited copies of the gene was removed (a partial ATXN1 knock-out). Each of these groups of mice was then compared to healthy control mice that do not have SCA1. The researchers found that mice with a very long polyQ expansion (154Q mice) performed poorly in both cognitive tests compared to healthy mice. The 78Q mice with a mild polyQ expansion did not behave differently from healthy mice, suggesting that cognitive symptoms may occur along a spectrum that correlates with polyQ length. This is consistent with how motor symptoms in mice and humans with SCA1 appear based on polyQ length.
To determine whether the cerebellum specifically contributes to the cognitive impairments in SCA1, Asher and colleagues subjected the Purkinje neuron-specific 82Q mice to the same cognitive tests. The authors found that the 82Q mice exhibited cognitive deficits similar to the 154Q mice. However, the 82Q mice were slightly less impaired than the 154Q mice. The authors concluded that Purkinje cell dysfunction is partially, but not completely, responsible for the observed cognitive deficit. This is an exciting finding because it highlights how the cerebellum is involved in both the motor and cognitive deficits seen in a mouse model of SCA1.
Asher and colleagues also explored whether mice without ATXN1 exhibit cognitive deficits using their behavioral assays. They compared the performance of animals with ATXN1 either partially or fully knocked out, to the performance of healthy mice. In both cognitive tests the researchers observed that animals with a partial ATXN1 knock-out performed similarly to healthy mice, while complete knock-out of ATXN1 caused worsened cognitive performance compared to the other two groups. These findings highlight how normal ATXN1 is important for cognitive performance
In summary, Asher et al. were able to recreate the cognitive deficits seen in some human SCA1 patients by using SCA1 mice. Their results demonstrate that these cognitive deficits are not artifacts of the genetic background, age of mice, or type of behavioral test used. Further, the authors demonstrated that the cerebellum does indeed contribute to the cognitive symptoms of SCA1 mice. More generally, these authors illustrated how the humble laboratory mouse can be a valuable asset to explore processes as complex as cognition in the study of human diseases. The careful evaluation used by Asher et al. helps to strengthen the foundation of scientists’ use of mouse models to study disease. When animal models better represent a human disease, we can ensure that our research is going in the right direction to find effective treatments and improve the lives of these patients.
Key Terms
Ataxia: A loss of muscular control, leading to abnormal walking, speech changes and irregular eye movements.
ATXN1: Ataxin-1 (abbreviated as ATXN1) is a small molecular machine known as a protein. Its function is to guide the creation of other proteins from our DNA blueprint, making it an incredibly important indirect player in a variety of cellular processes. When the gene encoding ATXN1 undergoes a rare mutation that elongates the resulting protein, the result is SCA1.
Cerebellum: A primary area of pathology in the spinocerebellar ataxias. This brain region sits toward the back of the skull and, though small in stature, contains the majority of the nerve cells (neurons) in the central nervous system. Contains the circuits that fine-tune our movements, giving us the ability to move with precision.
Cognition: The combination of mental processes that make up how individuals understand, learn about, and interact with the world. This includes processes like attention, learning, planning, and memory.
Gene: A unit of heredity made up of DNA that fully or partially controls the development of specific traits.
Mouse Model: A type of animal model with specific characteristics that allow for the study of various aspects of a human disease/condition.
Polyglutamine Expansion Disease / CAG-repeat diseases: A family of diseases caused by an expansion of glutamine amino acids in certain proteins.
Purkinje Neurons: A type of neuron in the cerebellum. They are some of the largest cells in the brain. They help regulate fine movement. Purkinje cell loss/pathology is a common feature in cerebellar ataxia.
Spinocerebellar ataxia (SCA): A group of heritable, adult-onset degenerative disorders. Please see our What is Ataxia? page for more details.
Conflict of Interest Statement
Marija Cvetanovic, who completed the work described in the summary, is a contributor to SCAsource. Marija Cvetanovic did not have any contribution to the writing or editing of this summary.
The author and editor declare no conflict of interest.
Citation of Article Reviewed
Asher, M. et al. Cerebellar contribution to the cognitive alterations in SCA1: evidence from mouse models. Human Molecular Genetics, 2020. 29(1) 117-131. (https://www.ncbi.nlm.nih.gov/pubmed/31696233)










