Written by Dr. Ambika Tewari Edited by Dr. Gulin Oz
Neurofilament light chain could provide a reliable readout of how far an SCA3 patient’s disease has progressed
How often have you heard that the most effective way to treat a disorder is early intervention? In reality, “early” is not possible for many disorders because patients receive a diagnosis only after the appearance of symptoms. But what if there was a way we could tell that a patient will develop a disease – even before they have any symptoms? Thankfully, that’s exactly what researchers in the field of biomarkers are trying to do. Biomarkers are biological indicators that are not only present in patients before the manifestation of symptoms, but can also be used to measure disease progression. In the SCA field, there have been a recent series of articles that have shed light on a promising biomarker for SCA3.
Spinocerebellar ataxia type 3 (SCA3), also known as Machado-Joseph Disease, is the most common dominantly-inherited ataxia. It is caused by an expansion of CAG repeats (a small segment of DNA that codes for the amino acid glutamine) in the ATXN3 gene. An important feature of SCA3, as well as in other spinocerebellar ataxias, is the progressive development of symptoms. Symptoms usually occur across decades, and can be divided into three major phases: asymptomatic, preclinical, and symptomatic. In the asymptomatic phase, there is no evidence of clinical symptoms (even though the patient has had the SCA-causing mutation since birth). In the preclinical stage, patients show unspecified neurological symptoms such as muscle cramps and/or mild movement abnormalities. By the symptomatic (i.e., clinical) stage, patients have significant difficulty walking.
Currently in SCA research, disease progression is measured using the Scale for the Assessment and Rating of Ataxia (SARA). A score of 3 or more on the SARA differentiates clinical and preclinical groups. Structural and functional brain imaging methods (such as MRI) also track the progressive nature of the disease, like the SARA, but give us a visual picture of changes in the brain. Together, these methods have provided the SCA community with important insights into the clinical spectrum of each specific disease and its rate of progression. And, with the exciting progress we have recently made in the realm of SCA3 therapeutics, a biomarker that is cost-effective and easy to measure (like in a blood test) could provide a convenient way to assess how effective a potential treatment is.
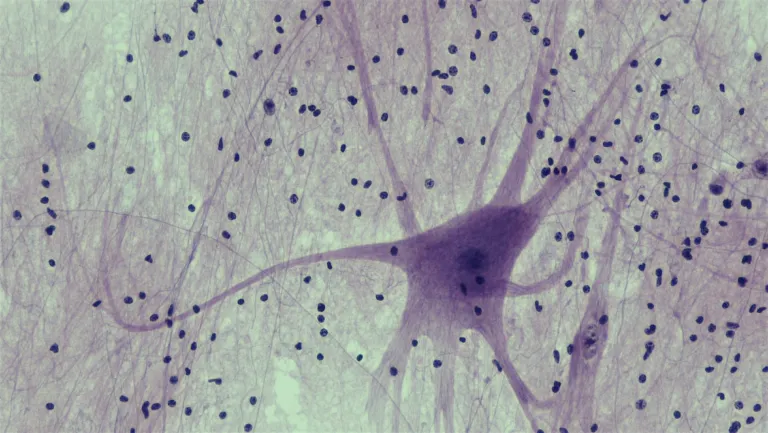
Two recently published studies have provided promising data on a potential SCA3 biomarker: Neurofilament light chain (NfL). Neurofilaments are an important structural component of neurons; in fact, research has shown that damage to neurons can cause an increase in the levels of neurofilament. It may come as no surprise, then, that NfL is being explored as a biomarker in many other neurodegenerative disorders.
When it comes to SCA3, though, it was a team led by Li et al that brought NfL to the forefront. In their study, the researchers had one group of healthy subjects (a “control” group) and one group of patients with SCA3. In both these groups, they compared the levels of NfL in the blood versus the cerebrospinal fluid (CSF), which is a blood-like fluid that surrounds the brain and spinal cord. The researchers found that patients with SCA3 had elevated levels of NfL in both blood and CSF compared to control subjects. Because of this, they concluded that NfL levels could be measured by a simple blood draw rather than the more invasive lumbar puncture (i.e., a spinal tap) to obtain CSF.
One of the crucial features of a biomarker is that it can accurately measure the progression of a disease. To address this, Li et al worked with a second group of SCA3 patients that were classified into either preclinical and clinical stages. Again, they measured levels of NfL in blood, but this time they correlated them with the patients’ SARA score. They found that blood NfL levels progressively increased from the early preclinical stage to the late preclinical stage, as well as from the preclinical stage to the clinical stage. After that, though, more advanced stages of SCA3 could not be distinguished by blood NfL levels.
These patients also received MRIs to measure the volume of their brains – specifically in the regions that are affected by SCA3. Higher NfL levels were associated with a smaller cerebellum and brainstem, which are two regions that undergo progressive degeneration in SCA3. These results showed that blood NfL levels were also capable of reflecting the level of brain loss (or “atrophy”) in patients.
After this study, an independent group enrolled even more patients and confirmed that there is a correlation between blood NfL levels and SCA3 symptom severity. This group, led by Peng et al, also included an asymptomatic group. These patients had an average of 70 CAG repeats in the ATXN3 gene, which is similar to the preclinical and clinical groups, but they had no movement symptoms. Interestingly, asymptomatic subjects also showed an elevation in NfL levels compared to healthy controls. This shows that, even before the onset of observable symptoms, changes in the brain are occurring. Furthermore, this study also showed a correlation between elevated NfL levels and an increased number of CAG repeats in the ATXN3 gene – a finding that typically corresponds to more severe symptoms and an accelerated disease progression.
For clinicians and patients, diagnosing a disorder in its earliest stages usually leads to better outcomes after treatment. The two studies described above used a large cohort of test subjects and careful analysis to show that increased blood NfL levels can predict SCA3, even before symptoms appear. Additionally, NfL levels can accurately predict the severity of SCA3 symptoms. Because of this work, NfL will serve an essential role in early detection and in clinical trials (i.e., to measure the effectiveness of new therapies as they come out). Still, further studies will be needed to determine why NfL levels do not reflect the progression of symptoms beyond early disease stages. Such experiments might even lead us to develop additional biomarkers that can be used throughout the entire duration of SCA3.
Key Terms
Neurofilament light chain (NfL): Definition
MRI: MRI scans are often used to image the brain to detect signs of ataxia, especially in a region of the brain known as the cerebellum. Ataxia often results in brain cell loss, and appears as reduced volume of brain tissue in the MRI image.
Biomarker: Any biological-based measurement that provides useful information regarding a person’s health. For example, blood test results showing increased glucose levels can be used as a biomarker for diabetes.
Asymptomatic: When someone has a condition, but no outward signs or symptoms. For folks with SCA3, although the disease causing mutation is present from birth, there is a period of time before symptoms begin to show. This time is called the asymptomatic phase.
Conflict of Interest Statement
Ambika Tewari and Gulin Oz have no conflicts of interest to declare.
Citation of Articles Reviewed
Li, Quan-Fu et al., Neurofilament light chain is a promising serum biomarker in spinocerebellar ataxia type 3. Molecular degeneration, 2019. 14:39 (https://doi.org/10.1186/s13024-019-0338-0)
Peng, Yun et al., Association of serum neurofilament light (sNfL) and disease severity in patients with spinocerebellar ataxia type 3. Neurology, 2020. (https://doi.org/10.1212/WNL.0000000000010671)









